ARTERY SURGERY
TCA CORONARY ANGIOPLASTY (TRANSLUMINAL CORONARY ANGIOPLASTY):
Many technical and material advances have been made.
Interventional cardiologists have acquired extensive technical experience enabling them to treat lesions that were previously complex and difficult, such as left main coronary artery stenosis, stenosis of bifurcations, and chronic occlusions, which are accessible by anterograde or retrograde approach.
The procedures are currently very predominantly (90%) by limiting radial arterial pathway, particularly hemorrhagic complications.
In terms of material, three types of procedures have been adopted:
1 - FFR (Fractional Flow Reserve)
It makes it possible to measure coronary artery reserve and evaluate significant stenosis.
2 - IVUS (Intravascular Ultra Sound) and OCT (Optical Coherence Tomography):
Endovascular ultrasound (IVUS) and optic coherence tomography (OCT) are two tools for the analysis of coronary atherothrombosis, and have become reference imaging of artherothrombose since the early 1990’s, for the analysis atheroma plaques and stent control.
Intravascular ultrasound (IVUS) and OCT (Optical Coherence Tomography) have made it possible
-
to obtain precise details on the degree and type of stenosis using direct imaging.
-
to visualize thrombus and dissection
-
to check the correct deployment of a stent and its correct affixation to the wall
3 - DCB (Drug-Coated Balloon):
“Treated” drug-eluting balloons make it possible to open intra-stent stenosis.
without adding intracoronary metal (a new stent).
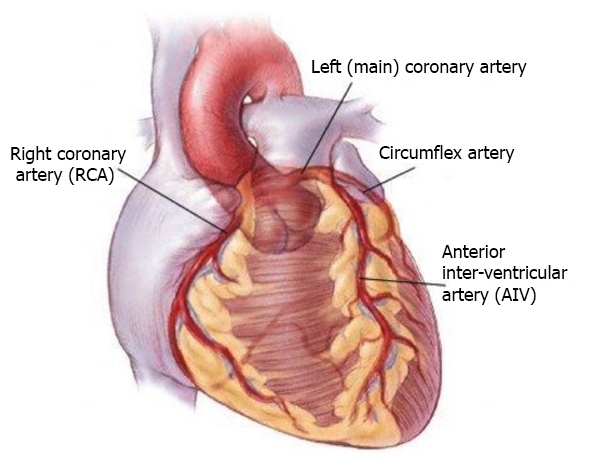
CORONARY ARTERY SURGERY:
Coronary artery surgery in turn has made advances over the last few years as follows:
1- Technical advances:
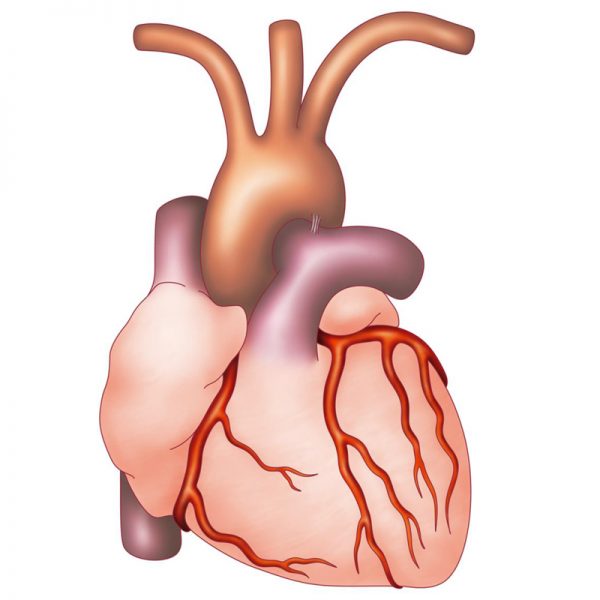
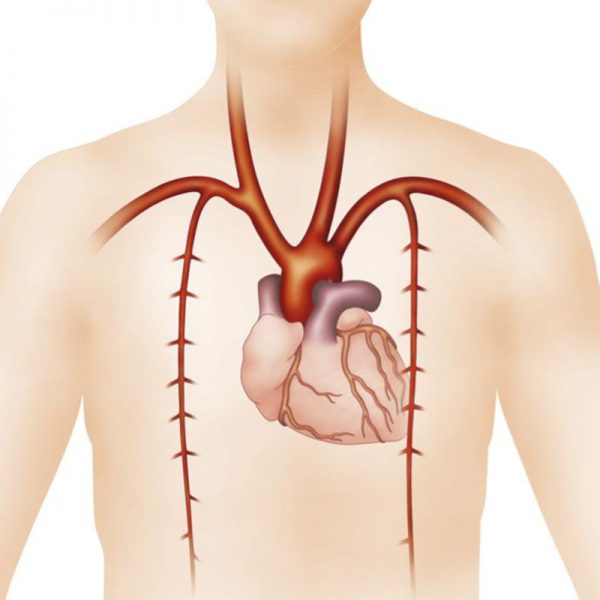
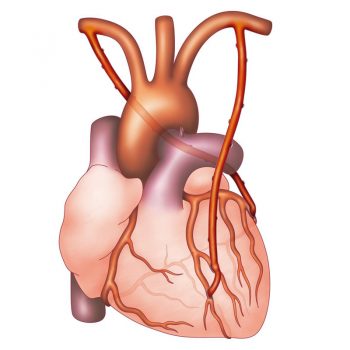
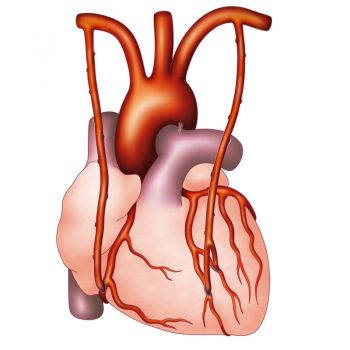
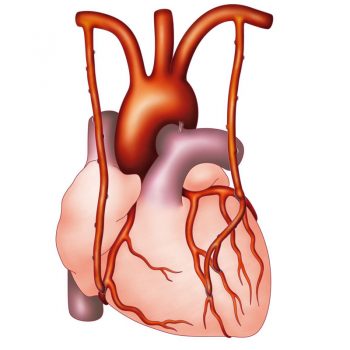
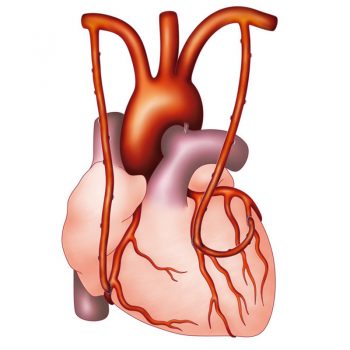
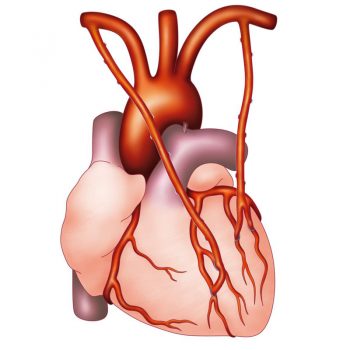
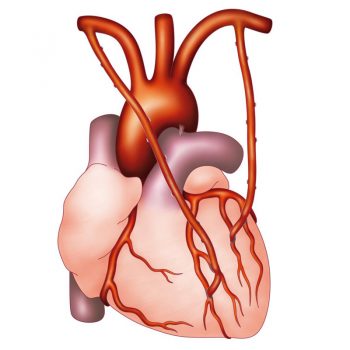
Systematic use of 2 mammary artery grafts (Total arterial coronary bypass).
The 2 Internal Mammary Arteries are two excellent arterial grafts, whose anatomical structure and calibre are identical to that of the coronary arteries. This accounts for their longevity in comparison to other types of grafts: veins, radial artery…
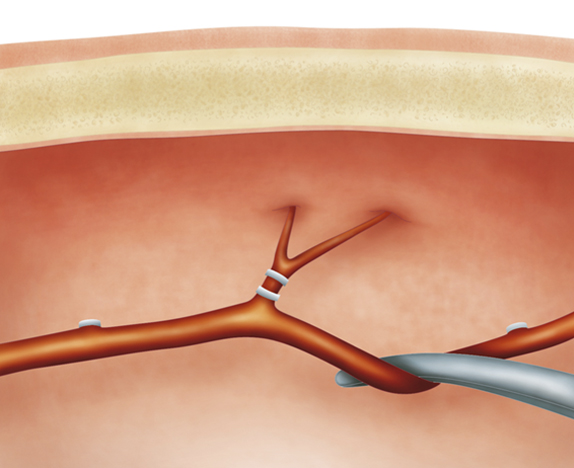
For Pr Khoury and according to his experience, the two “pediculated” internal mammary artery grafts (i.e., not sectioned, used as a free graft or as a “Y” graft) make it possible to perform, in almost all cases, a so-called complete and “Anatomical” revascularisation. This also takes into account anatomical variations by favouring the dominant coronary artery network and the patient’s coronary artery lesions.
The diagrams above show us the different possibilities.
See article “Anatomic coronary revascularisation” and the link.
The left mammary artery is anastomosed on the IVA and the laterally lateral diagonal
The right mammary artery is anastomosed directly on the lateral passing behind the Aorta.
The mammary left is anastomosed on the IVA and the diagonal using the natural bifurcation of the graft.
The mammary right is anastomosed directly on the right coronary
The mammary left is anastomosed on the IVA laterally laterally (in kissing) then the lateral
The mammary right is anastomosed directly on the right coronary
The mammary left is anastomosed on the IVA laterally laterally (in kissing), then the lateral.
The mammary right is anastomosed directly on the right coronary
The mammary bifurcation left is anastomosed on the lateral 2,
The right mammary artery is anastomosed on the IVA and the diagonal.
2 – Advances in the medical-surgical field.
We have made great strides in peri-operative surgery. Improved pre-operative preparation of patients, anaesthesia and intensive care measures have become safer, management of post-operative functional rehabilitation has become better targeted, currently enabling increasingly less invasive surgical procedures.
1-Management of the patient:
Improved patient management cardiologists has enabled us to have patients who are medically stable, with diabetes well under control, keeping in mind that one third of coronary artery patients are diabetic.
The different cardiovascular risk factors (arterial hypertension, hypercholesterolaemia and other factors, etc.) are increasingly better treated.
The pre-operative assessment has become very rigorous, even comparable to an airplane pilot’s check-list: the patient cannot undergo surgery before a series of tests are performed such as pulmonary function tests (PFT), vascular investigation with doppler ultrasound, detection of possible infection by means of urinalysis, ENT, dental and respiratory assessments.
2 – Anaesthesia:
The pre-operative consultation in anaesthesia is compulsory. Different anaesthetic techniques enable major peri-operative stability and a faster and safer regain of consciousness.
Anaesthesiologists have new techniques to introduce catheters via ultrasound/doppler method, video monitoring for difficult-to-perform intubation, and peri-operative echocardiography for better controlled conduct of surgery.
Anaesthetic products are less aggressive and of shorter duration.
3- ECC (extra corporeal circulation):
Use of new techniques of ECC, such as mini ECC, also called MAC, has made it possible to significantly decrease the aggressiveness of conventional ECC on components of the blood and, by the same token, to simplify post-surgical follow-up.
The pump off procedure is also a technique which makes it possible to perform bypass grafting on the beating heart without ECC.
La pump off est aussi une technique qui permet de réaliser des pontages avec un cœur battant sans CEC.
4- Post-operative intensive care:
Extubation can be performed faster.
ECMO (extracorporeal membrane oxygenation) circulatory assistance and systematic repeat ultrasound examination are high performance tools in the hands of intensivists.
5- post-operative functional rehabilitation:
Currently, rehabilitation now makes possible faster recovery, which is also less painful and less invasive.